This page has information about COVID-19 and how you can continue your recovery both in the hospital and once you return home.
The Corona Virus (COVID-19) tends to affect a person’s airways and can cause shortness of breath, coughing, fever and the oxygen levels in the blood to decrease.
It is transmitted person to person through airborne droplets produced when a person coughs or sneezes. It can also be transmitted through touching a surface that an infected person has previously touched.
The virus generally lasts between 2-14 days.
Hand hygiene
Hand washing is a vital tool to prevent the spread of Corona Virus. Listed below are some tips to ensure effective hand washing.
- Wash your hands with soap and warm water for at least 20 seconds regularly
- If soap and hot water are not available, use hand sanitiser
- Wash your hands when you return home
- Use a tissue or sleeve to cover your mouth and nose when sneezing
- Immediately put any used tissues in the bin and wash your hands afterwards
- Do not touch your face without washing your hands
Treating breathlessness and fatigue
Pacing – This helps to manage feelings of fatigue and will allow you to conserve energy throughout the day.
Tips for pacing include:
- Prioritising activities throughout the day
- Taking frequent breaks
- Try not to talk and move together
Give yourself time to recover your breath
Positioning – The muscles in the shoulder & neck are the same muscles that assist with breathing When becoming short of breath, certain positions can be used that help to support your neck & shoulders so that these muscles can be used solely for breathing.
Breathing Techniques – ACBT
ACBT (Active Cycle of Breathing Technique) is used to assist with loosening and clearing mucus as well as, improving ventilation in the lungs and your coughs efficiency. There are 4 stages of ACBT:
Breathing Control – Gentle, normal breathing using your stomach. With your hands placed on your stomach, you should feel your hands rise as you breathe in & fall as you breathe out. Breathing should be slow and steady.
Deep Breaths – Focus on a slow deep breath in through your nose, hold your breath for a count of 1-3 seconds and breathe out gently through your mouth.
Huffs – Take a big breath in through your mouth, keeping your mouth open; imagine trying to steam up a mirror with force and huff all the air out. (Breathing control should be used between huffs to avoid becoming breathless).
Cough – If you feel that you have phlegm to clear from your chest, try having a big strong cough. If you have no phlegm to cough up focus on the cycles of breathing control and deep breathing.
Bed Exercises
Although you may feel tired, these basic exercises can benefit your recovery. Start with 6-8 repetitions and increase to 12 over time.
Start by pointing your toes to the end of the bed and back to the ceiling.

With a rolled up towel under your knee lift your heel off the bed.

Push your knee down into the bed.

Bring your heel up the bed toward your bottom.

Bend your knees and lift your bottom off the bed.
Chair Exercises
Being sat out in a chair will have a positive effect on your lungs, muscles, digestive system & circulation.

Marching on the spot

Straighten on knee and hold for 3-5 seconds.

Cross arms and turn to the left & right.

Bend your elbow to your shoulder, then straighten.

Lift 1 arm above your head and slowly lower.

Keep elbows at your side & move arms out.
Standing Exercises
Ensure you have a firm surface to hold (e.g. a kitchen work top). Exercises can be done throughout the day rather than all at once to make them more manageable.

Take leg out to the side & return to centre.

Move up onto tip toes & gently lower back down.

Move leg out behind you & gently back in line.

Bend knees as able, slowly push back up.

Marching on the spot.
Sit to stand - push up with hands if needed.
Being discharged from hospital
Upon discharge you should be active on the ward completing your normal daily activities (getting washed & dressed, toileting). Any difficulties can be discussed with your therapy team.
During your stay in hospital, your usual medication may have been altered. Prior to discharge you will be provided with a supply of medication and instructions, your GP can prescribe the medications required. If you have any concerns, these can be discussed with your doctors.
If family or friends are unable to come and collect you from hospital, alternative transport can be arranged after discussion with your nursing staff.
Isolation guidelines
How long before I can go outside?
Current guidance is for a symptomatic person to self-isolate for 7 days however, due to time spent in hospital, it is advised to self isolate for 14 days after the onset of symptoms. This is due to the higher viral load experienced by those admitted to hospital causing them to be contagious for longer.
Please discuss with your doctor if you have any questions.
Physical Activity at Home
Getting moving will help continue your recovery once home. Getting out of bed, washed & dressed, having breakfast then sitting in a chair will help to start building strength and helping you feel better.
Important considerations prior to exercise.
During your stay in hospital your body will have used a lot of energy to fight the illness, the body will have gained some of this energy from its stores in the muscles. This combined with decreased activity levels will have caused your muscles to become smaller and weaker.
Due to this daily activities may feel that they are more tiring and feel harder to complete than they did previously. Some patients have found that this causes them to become more inactive, or they would do lots of activity on one day but then have a flare up of weakness or pain and have to rest for a coupe of days.
This can be frustrating however, pacing yourself & doing jobs or activities little and often will help you recover.
Exercises at Home
Start your exercises by doing 6-8 repetitions and gradually increase this to 12 over time.
Try and complete the exercises 2-3 times per week to help improve your strength and balance.
Guide to Physical Activity
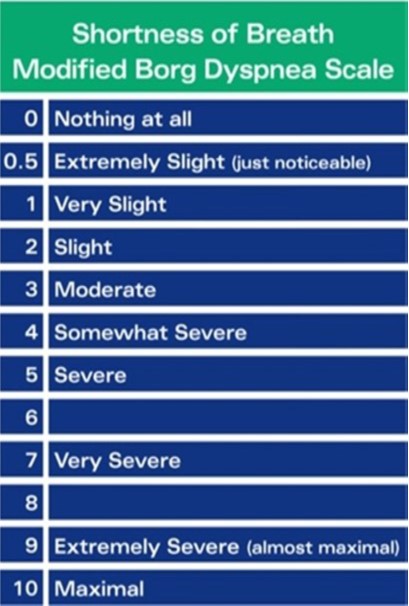
This scale allows you to rate the difficulty of your breathing. It can be used to monitor how breathless you feel when exercising. This can be used to show how your lungs are improving. It is important that you take regular rests and stop before becoming too short of breath. You should aim to be between zones 3-5 when exercising.
When exercising it is normal to feel out of breath & your heart rate to increase. This should return to normal within 5 minutes of resting.
Exercise done at a moderate level helps to increase endurance and lung function.
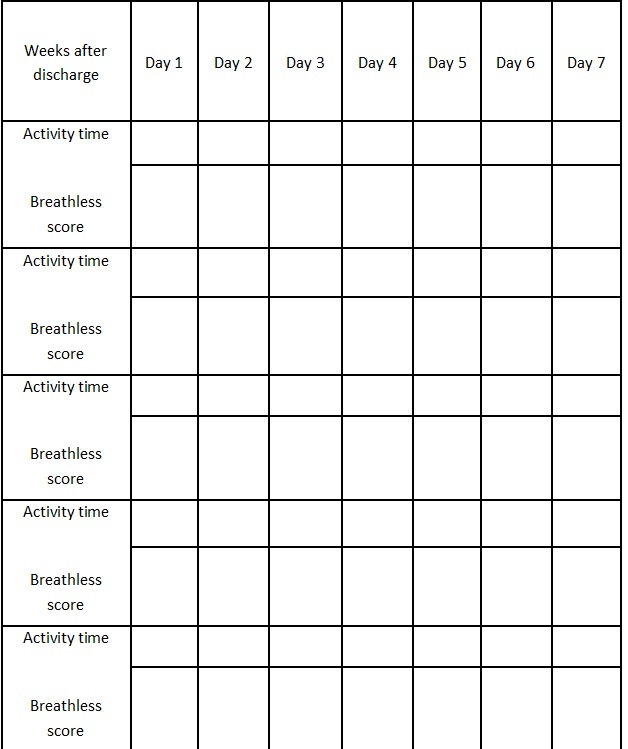
You can record your scores using the table on the next page, by doing this you should note an improvement over time.
Exercise/Activity Log
Nutrition and covid-19
Covid-19 can affect people in different ways. If you have recently had covid-19, you may be feeling weak, tired, breathless, had a poor appetite or taste/smell changes. These symptoms can affect your nutritional intake, make tiredness worse or could cause weight loss. It may also be that you have found it difficult to manage your long-term health condition and your nutrition can help to manage these problems. A healthy balanced and nourishing diet will help to give you more energy, build a strong immune system, manage your weight, and rebuild muscle and strength.
Alongside exercise, protein is especially important to build muscle and strength, because it is difficult to gain muscle without enough protein. Focus on having a protein source with each meal, as well as some high protein snacks in between. Each meal should have either: meat/chicken, fish, eggs, beans, lentils, tofu or other meat alternatives. High protein snacks include cheese, cold meats, nuts and nut butters, thick yoghurts, protein bars etc.
Weight loss is often seen as a positive change but if you are unwell with covid-19 and less active, you may lose muscle mass and strength so it is important to try to eat well to maintain your strength during recovery. Weight loss should only be attempted once you have recovered fully.
With all the symptoms of covid-19, it can be difficult to eat enough, let alone eat healthily. It is often helpful to have a little and often approach to eating which means having small portions of easy to eat foods regularly throughout the day. With breathing difficulties and a reduced appetite it can be easier to have soft or liquid foods such as custard, rice pudding, yoghurt, and milky drinks.
If you are only managing to eat small portions of your meals, you can increase the calorie and protein content of your food by fortifying meals with grated cheese, add peanut butter to porridge and toast, mix double cream into soups, add dried milk powder into hot drinks puddings or soups, etc. Taking some nutritious drinks, such as milkshakes, may also be helpful. If you have followed this advice and continue to eat less, lose weight or concerned about your diet, you can do the self-screening for malnutrition below to see if you should get some more help from a dietitian.
Vitamins and minerals are essential for a healthy functioning immune system. You can make sure you are getting enough by having a variety of 5 portions of fruit and vegetables a day. This also gives you fibre to aid digestion, cardiovascular health, and manage sugar levels. Have them in a salad, as a snack, add them into sauces and stews (fresh, frozen, or tinned all count).
Vitamin D is particularly important in protecting muscle, bone health and supporting the immune system. If you do not spend much time in the sun, consider taking a daily 10 microgram vitamin D3 supplement, especially in the colder months. To find out if you are at risk of a deficiency, visit the NHS website’s page on vitamins and minerals.
For more details about the topics mentioned above and for advice on specific symptoms, you can visit these sites:
- To complete the self-screening for malnutrition, type: “Patient nutrition checklist” or “Malnutrition self-screening” into a Google search.
- For advice on eating more with a small appetite, type: “BDA fact sheet malnutrition” into a Google search.
- For advice on eating during Covid-19, type “BDA malnutrition pathway covid patient leaflet” into a Google search and choose the leaflet that suits your needs.
- For advice on eating for recovery after critical illness, type: “BDA nutrition at home after illness” into a Google search.
- For advice on specific symptoms related to covid-19, type: “BDA Tips to help with eating problems” into a Google search.
- For a video version of dietary advice for covid-19, type: “Patient webinars covid-19”
- For advice on diet and fatigue, type: “BDA chronic fatigue” into a Google search.
- For dietary sources of protein, type: “managing malnutrition: protein foods” into a Google search.
- For more detailed information on vitamins and supplements, type: “NHS vitamins and minerals” into a Google search.
- To make a start on your weight loss journey, type: “NHS weight loss plan” into a google search.
If you have difficulty accessing any of these online resources, call the nutrition and dietetics department on 01935 384 250 and we can help guide you to the resources.
Relaxation & Mindfulness Techniques
Whilst exercising regularly is important, your body & mind needs time to relax and unwind.
Stress and anxiety are common after an illness and can cause:
- Increased heart rate & blood pressure
- Interrupted sleep
- Low mood making it difficult to resume normal activities
Guided imagery is a technique used in relaxation. It involves mentally visualising a place in your life that represents safety, comfort and/or happiness. This can include places such as a garden, beach or house. During this time you should attempt some deep breathing exercises, to aid in relaxation.
Whilst you have been unwell your body has been through a lot so it is important to make time to relax. It does not take long and can help reduce stress and anxiety levels.
Examples of mindfulness can be found on YouTube by searching ‘Every Mind Matters’
The easiest way to relax is to do something that you enjoy e.g.
- Listening to music
- Reading a book
- Sitting in the garden
- Drawing or doing something creative.
Anxiety
Everyone will experience anxiety during their lifetime and it is a very normal reaction when you are overcoming illness. Occasionally feelings of anxiety can be overwhelming and affect your daily life.
Anxiety can cause you to become sweaty, shaky, it can increase your heart rate and make you short of breath. It can also cause you to become overly careful or to avoid things that trigger the anxiety.
Follow Up After Discharge
Severe Covid Pneumonia will have a follow up telephone consultation 4-6 weeks post discharge, then a face to face clinic review at 12 weeks. At this appointment you will have a chest x-ray, spirometry to measure your lung function and a walk test to give an indication of your exercise tolerance. It will also be determined if further investigations are required.
You will receive a holistic needs assessment and will be provided with further information for any extra support you may need.
Mild/moderate Pneumonia you will be invited to attend for a chest x-ray after 12 weeks. Further information will then be sent if needed with a report of your chest x-ray, it is expected that many at this point will not need a further follow-up appointment.
If you have any further questions please ring Clare Genton—Senior Respiratory / Critical Care Physiotherapist on 01935 606578
Support Services
Spark Somerset
https://www.sparksomerset.org.uk/covid-19
Dedicated webpage and support line for community support during Covid-19.
Support line: 01460 202 970
The Sepsis Trust
COVID-19: Recovery Response
The Sepsis Trust have started a dedicated Covid-19 recovery response service. This service is available to anyone who has been ill in hospital and their families.
Their support team can be contacted by phone on 0808 800 0029 or online and via email through the above website.
Somerset County Council
https://www.somerset.gov.uk/coronavirus/get-help/
The Somerset County Council website has plenty of information regarding how to get help at home. They also have a Coronavirus help line: 0300 790 6275
Ref: 36/20/101
Review: 11/22










