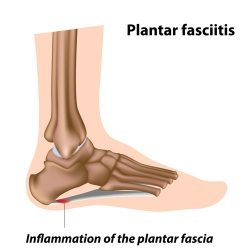
What is plantar fasciitis?
The plantar fascia is a band of fibrous tissue in the sole of the foot, running from the heel bone to the bases of the toes. It helps support the arch of the foot and acts as a shock absorber when walking.
Literally, plantar fasciitis is inflammation of the plantar fascia. With excessive stress on the plantar fascia, and or loss of its usual elasticity, small tears can occur in its fibres. This can result in pain and localised inflammation. Sometimes a spur of bone will form on the heel as a response to the repetitive pulling on the plantar fascia. This is a result of the condition rather than the cause of the pain.
The causes include:
- Excessive weight
- Unaccustomed increase in activity
- Inappropriate footwear
- Excessively high arched or flat feet
- Calf muscle tightness
What are the symptoms?
- Pain in the heel on the sole of the foot, sometimes also felt in the instep
- Pain worst on the first step in the morning and after getting up following a period of inactivity
- Pain aggravated by long periods of standing or time on your feet
What is the treatment?
The mainstay of treatment is a rigorous plantar fascia and calf stretching programme to lengthen the tight tissues, decreasing the tension and allowing healing. This is best coupled with silicone heel cushions (Viscospot) to protect the painful area.
The stretching may cause an initial increase in your symptoms but this will usually settle over the first week if you keep to the programme.
The majority of patients’ symptoms begin to improve within
one to two weeks of starting the treatment and the vast majority
will have improved significantly within eight weeks.
Other treatments you may also find helpful in combination with the stretching programme and heel cushions are:
- Non-steroidal anti-inflammatory tablets or locally applied gel
- Ice packs (a plastic bottle of water frozen and then rolled under the foot)
- Night stretching splints
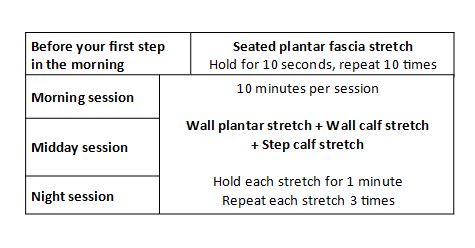
Seated plantar fascia stretch
Sit with your bare foot crossed over the opposite knee. With the hand of the affected side pull the toes and foot back towards the shin until you feel the stretch in the arch of the foot. To check that the stretch is correct, feel the taut plantar fascia with the opposite hand.
Hold this stretch for 10 seconds and repeat 10 times.
Wall plantar stretch
With your shoes on, stand facing a wall. Dig the heel of the
affected foot against the floor close to the wall, such that the undersides of your toes are against the wall with your toes bent backwards. Push the knee of the affected foot towards the wall. You should feel the stretch both in the arch of the foot and in the calf. Your knee should not be able to touch the wall.
To increase the stretch, move your heel closer to the wall and your toes further up the wall, again pushing your knee towards the wall.
Hold this stretch for one minute and repeat three times.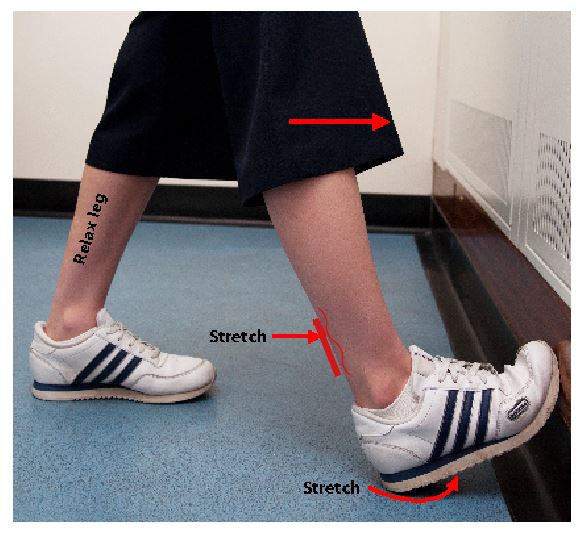
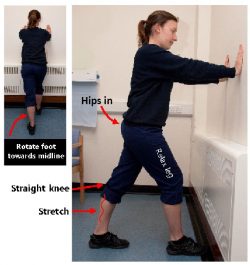
Wall calf stretch
Stand facing the wall with your hands resting on the wall in front of you at shoulder height. Reach the affected foot out behind you, with the toes pointing forwards towards the heel of the opposite foot, such that, with your knee completely straight, your heel can still just sit flat on the floor. Then bend the opposite knee, pushing forwards such that you feel a stretch in the affected calf.
Hold this stretch for one minute and repeat three times.
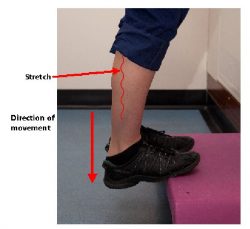
Step calf stretch
Stand with the balls of your feet resting on the edge of a step, holding on to something for balance. With your knees straight, allow your heels to sink below the step such that you feel a stretch in the calf.
Hold this stretch for one minute and repeat three times.
Initially you may find this is uncomfortable and you may only be able to do this by sharing the weight through each foot. With time, as you are better able to tolerate the stretch, you may find it better to perform the stretch on only the affected side, lifting the other foot into the air.
I’ve tried physiotherapy and insoles before and it didn’t work, why should this?
Not all stretching programmes and insoles are as effective. Until this treatment has been tried in full it is not possible to rule it out.
Should I continue to exercise?
Rest tends to allow the plantar fascia to tighten and has not been shown to resolve your symptoms faster. Running causes sudden impact and stress to the painful area with each step and is probably best avoided until your symptoms resolve. If you do choose to continue running, select soft running surfaces, wear your heel cushions and decrease the intensity of your training. Other non-impact exercise, such as swimming, cycling and cross-training are preferable as they cause less stress on the plantar fascia.
How long should I continue with the stretching programme and heel cushions?
Continue until your symptoms have fully resolved. If after stopping the treatment your symptoms begin to return, simply restart the programme until the symptoms resolve again.
What if my treatment fails?
If after three months of performing the stretches correctly and wearing the heel cushions consistently you have not improved, you will need further assessment and consideration of alternative therapy. This may include injections or heel shockwave therapy. Only very rarely is surgery required.
DiGiovanni, BF; Nawoczenski, DA; Malay, DP et al.: Plantar
fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am. 88:1775-1781, 2006.
Pfeffer, G; Bachetti, P; Deland, J et al.: Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int. 20:214-221, 1999.
If you require further information or advice, please contact:
Orthopaedic secretary: 01935 384 818








