Welcome
On behalf of the Orthopaedic Surgery team at Yeovil District Hospital, we welcome you.
This app has been developed to guide you through every step of your orthopaedics journey. The app will provide you with all the important information you require to navigate successfully through your surgery journey and beyond.
Orthopaedics at YDH
YDH has on of the best Orthopaedics surgery teams within the NHS. This experienced and dynamic team stops at nothing to ensure the success of your surgery.
Meet the YDH Orthopeadics team.
Information
The Orthopaedic Department is staffed by a multi professional team including Medical staff, led by the Clinical Director, Nurses, led by the Matron, Physiotherapists, Occupational Therapists and other supporting agencies.
Patient consent
Our commitment to you is to inform you of all aspects of the intended procedure you are to undergo. You will then be required to ‘consent’ in writing to your procedure. Following your individual consultation with your surgeon, should you wish for further clarification of any aspects of which you have been informed, please ask the nurse who will be happy to clarify issues.
Data Protection Act
Your name is entered onto our computerised database, enabling us to keep effective clinical records. Under the Data Protection Act you have the right to view any records held by Yeovil District Hospital. Please ask a nurse should you wish to access them. If you or your representative wish to have copies then you will have to give your written consent for a copy to be made. You will have to pay for this copy.
Chaperone
You have the right to have a chaperone provided by the Hospital, during any examination and certain procedures. You may choose a family member or close friend or carer. You also have the right to choose a carer to be involved in your care.
Smoking
Smoking is actively discouraged, particularly prior to and immediately post operatively, as this can add to complications of surgery. Yeovil District Hospital has a no smoking policy with which we request your co-operation. You may find it helpful to discuss giving up smoking with your doctor or practice nurse. Nicotine replacement therapy (patches or gum) may be considered, ideally four weeks prior to your admission to the hospital.
Dietary requirements
You will have a choice of meals to select from. If you have special dietary needs please inform a member of staff. Please feel free to remind the ward staff of your needs on your arrival.
Mobile phones
For the safety of all patients the use of MOBILE PHONES is restricted in some areas of the hospital and you may not be able to use your phone on the ward on which you are placed. Please ask the nurse in charge BEFORE you make a call.
Risk management
Yeovil District Hospital has comprehensive Risk Assessment Policies in place, which ensure that patients’ safety is assured and that areas of improvement are identified and an improvement plan implemented.
Manual handling policy
Yeovil District Hospital operates a Non Lifting Policy. Staff are available to assist your mobility needs and are trained in the use of equipment when it is required. Please ask if you need assistance to move.
Single-sex accommodation
Being in mixed-sex hospital accommodation can be difficult for some patients for a variety of personal and cultural reasons. Here at Yeovil District Hospital we understand this and strive to treat all patients in privacy and with dignity. For this reason, we have worked to ensure that we provide single-sex accommodation for all patients where ever possible. Privacy and dignity are at the heart of our policy and they are vital components of quality care. The over-arching goal is to deliver single-sex accommodation across the service, however the varied needs of different patient groups and clinical settings are recognised. There are occasions when mixed-sex accommodation is unavoidable, but patients’ privacy and dignity will always be assured.
Your surgery overview
Total hip replacement
The normal hip
The hip joint is a ball and socket joint between the top of the thigh bone and the pelvis which lies deep in the groin. It consists of a ball (femoral head) at the top of your thigh bone (femur) and a socket (acetabulum) in your pelvis. The surfaces of the ball and socket are covered by a smooth, low friction material called articular cartilage, which cushions the bones and lets them move easily. However, this can become worn and thin, a process known as osteoarthritis. Ligaments and muscles help keep the ball within the socket whilst allowing a large range of movement.
Hip function
The hip joint bears the full weight of your body. In fact, when you walk, the force transmitted through your hip can be up to three times your body weight. As well as transmitting weight, the hip needs to be able to move freely to enable you to function normally. Muscles surrounding the hip such as your buttock (gluteal) and thigh muscles (quads) are also important in keeping your hip strong and preventing a limp.
When the hip becomes arthritic
As we get older many people will develop “wear and tear” arthritis of the hip, although some will have rheumatoid arthritis which also involves other joints. Many factors may contribute to having arthritis; obesity, accidents, vigorous sport or a family history may all play a part. In osteoarthritis (wear and tear), certain changes occur in the joint.
- The smooth cartilage becomes flaky and develops small cracks.
- The bone underneath the cartilage becomes denser.
- The lining of the joint becomes inflamed and may thicken up.
As the arthritis progresses, there may be:
- Severe wear of the cartilage allowing the bones to rub and grate together.
- Loss of the joint space.
- Formation of bony lumps called osteophytes.
The artificial joint
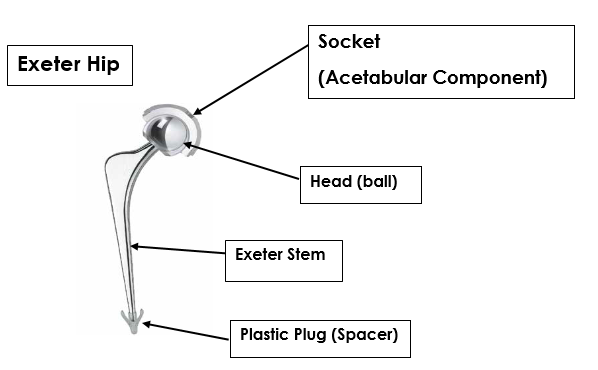
The worn part of your hip joint is replaced with an artificial joint made of surgical quality stainless steel, a metal alloy or ceramic. A plastic (polyethylene) liner is usually used. Some can be used with orthopaedic cement; others have a special coating that binds with the bone instead. Your surgeon will choose the most appropriate type of hip replacement for you. A total hip replacement is made up of the components shown here.
Why do I need a hip replacement?
- Because you may have pain which at times is severe and disabling which makes it difficult or impossible to carry out normal daily activities.
- You cannot walk very far now and may have to use a stick. Stairs can be very difficult.
The main reason for recommending a hip replacement is pain or loss of function due to arthritis. The aims of the hip replacement are to relieve the pain from your hip and to enable you to carry out your normal activities more comfortably.
The operation
A hip replacement is a major operation. You will spend 3-4 hours in the operating department. The operation itself will take 1-2 hours.
- The femoral head is removed
- The natural hollow in the pelvis, called the acetabulum, is hollowed out and a socket is fitted into the hollow
- A metal stem is secured into the canal of the thigh bone
- The cup and the metal stem may be either press-fit or may be fixed with acrylic cement
- The layers of soft tissue, muscle and skin are stitched and clipped back together
You are usually in hospital for two – four nights. You should be prepared to work hard at the exercises given to you by the therapy staff. Most patients tell us that they are pleased with the result of their hip replacement. Some, however, are less satisfied either because a complication has arisen or their expectations are too high.
Video and pathway
Preparation
Preparing your home
Arranging some support for when you return home
If you have not already done so, please start thinking about when you go home and start to organise and make the necessary arrangements.
These are the things that you need to consider:
Many patients find it helpful if friends or relatives come to stay, or they go and stay with them following your discharge from hospital.
Convalescence is not funded by the hospital or social services, you may be able to arrange this privately. Home care is limited and the need is assessed on an individual basis. You need to consider how you will manage any caring responsibilities you have (including pets), shopping, laundry and meals.
Preparing your home for your return
It is very important that your home situation is suitable for you to return to following your surgery, especially if you live alone. Here are some things you should do:
- Clean and do the laundry and put it away.
- Put clean sheets on the bed.
- Prepare meals and freeze them or buy ready meals that are easy to prepare.
- Pick up loose rugs and mats.
- Make sure there is room to walk from room to room without obstacles getting in your way.
It is your responsibility to ensure you have suitable transport for your admission and discharge home.
Instructions for surgery
What to pack and bring into hospital
Pack a small bag of clothes and other items (see check list below).
Please bring with you any medication that you are taking in the original containers. There is very limited storage space on the ward so please bring your belongings in a soft sided holdall in preference to a suitcase.
- Your Hip Replacement Guidebook
- Footwear: Slippers - not mules. Trainers/flat shoes, preferably slip on
- Aids: Walking sticks or frame, crutches, dressing aid
- Nightwear: Dressing gown, nightdress/pyjamas
- Daywear: Loose fitting day clothes
- Toiletries and towels. Tissues and wet wipes
- Money: Small amount for newspapers, magazines. Please do not bring credit or debit cards with you
- Books/magazines
Reducing the risk of infection in hospital
What you can do to help?
- Keeping your hands and body clean is important when you are in hospital. Take personal toiletries including soap and a clean flannel with you.
- Taking a container of moist anti-bacterial hand wipes with you will ensure you always have some available when you need to clean your hands, for example immediately before you eat a meal.
- Ensure you always wash your hands after using the toilet and if you use a commode.
- Hospital staff can help protect you by washing their hands, or by cleaning them with special alcohol rub or gel. If a member of staff needs to examine you or perform a procedure, e.g. change your dressing, do not be afraid to ask if they have first washed their hands or used an alcohol rub or gel.
- Try to keep the top of your locker and bed table reasonably free from clutter. Too many things left on top make it more difficult for the cleaning staff to clean your locker and bed table properly.
- If you visit the bathroom or toilet, and you are concerned that it does not look clean report this immediately to the nurse in charge of the ward. Request it be cleaned before you use it, and use an alternative in the meantime.
- Your bed area should be cleaned regularly. If you or your visitors see something that has been missed during cleaning report it to the nurse in charge and request it is cleaned.
- Always wear something on your feet when walking around the hospital.
- Ensure your visitors use the hand gel on arrival to and departure from the Ward.
- Please make sure that if your visitors are feeling unwell or have had diarrhoea and or vomiting in the last 48 hours they must stay away from the hospital.
- Visitors must not sit on the beds and are requested to use the chairs provided.
Preparation for your hospital stay
Do as much moderate exercise as your pain will allow, but in particular make sure that you do the pre-surgery exercises you have been given.
Stop smoking – your chest needs to be clear for your anaesthetic.
Drink alcohol only in moderation.
Good nutrition will improve your recovery and will be part of your treatment whilst in hospital. Eating a varied, healthy and balanced diet will ensure that your nutritional needs are met. This is essential both before and after your operation.
Healthy eating
If you are overweight and your consultant has recommended that you lose weight before your operation it is best to eat a varied healthy diet. This will help maintain your vitamin, mineral and protein levels which is ideal for an operation.
If you want more detailed information please see the NHS Choices website or ask your GP to refer you to a community dietician.
General healthy eating advice
Eat more fruit, vegetables and cereals. Fruit, vegetables and cereals are all rich in vitamins and fibre (roughage). All fruits, vegetables and salads are beneficial and you should try and have five portions a day. Wholemeal/ wholegrain foods like wholemeal bread/pasta/rice, porridge, Weetabix and other high fibre cereals, beans, lentils and oats are also good for you to try and keep healthy.
Eat less fat
Grill, poach, bake or steam food, instead of frying or roasting. Eat more fish and poultry (remove the skin). Choose lean cuts of meat and trim off all the fat you can. Use skimmed or semi-skimmed milk and try low-fat yoghurt and margarine. Avoid high fat ‘take-aways’ for example; burgers, fish and chips, sausages and oily Indian foods. Avoid crisps chocolate, and biscuits as these are also high in fat.
Cut down on sugar
Sugar contains no useful nutrients apart from energy and we can get all the energy we need from other foods. Reduce your intake of sweets and limit adding sugar to foods and drinks. Reduce sugar containing drinks.
Alcohol
Limit the amount of alcohol to 14 Units for women and 21 units for men a week and try and have 2 days free on alcohol in each week. Alcohol contains calories and having too much can cause more health problems.
For information on what a unit is please ask any health care professional.
Build up advice for those not eating well or with a low body weight
During an illness or debilitation you may require additional nutrients. In such an event, a high protein and energy diet is required to maintain weight and muscle mass, rather than a low-fat diet.
If you have lost weight recently, please ask your nurse for a ‘Have you got a small appetite?’ leaflet for help and advice.
Your dietician or doctor may prescribe nutritional drinks for you if you have a low body weight or are not eating well. Please ask for a referral to a dietician if you have any concerns.
Consent information
Consent information can be found at the following link. https://yeovilhospital.co.uk/patients-visitors/consent/
We ask patients to sign a consent form prior to surgery, and on the day of surgery. The consent document can be found here for reference. https://yeovilhospital.co.uk/wp-content/uploads/2021/08/Consent-Form-1.pdf
Pre-assessment
Today you attended a Pre-assessment Clinic appointment
As far as can be assessed, you are fit for surgery, however you will be contacted if any of your test results are abnormal and need to be followed up. This may mean your operation or procedure needs to be postponed, but you will be advised on the way forward.
If you develop any illness or infection, or experience any changes in your health prior to your operation/procedure please contact the Pre-assessment Clinic on 01935 384863. They will be able to advise you whether your operation will be able to go ahead, after discussion with the anesthetist and/or surgeon.
Sleeping
Ensuring you are getting an adequate amount of sleep is important in the preparation for your surgery.
Fasting
7:30am/8am admission - for surgery on the same morning
Do not eat anything AFTER midnight, or have milk, on the day of your operation.
You can drink water up until 6am and then nothing to drink after this time. Prescribed drinks for enhanced recovery should be taken in accordance with the guidelines given to you by the Preassessment Clinic staff.
Please do NOT chew gum, eat sweets or drink anything other than water. ALL other fluids, including tea, coffee, carbonated drinks eg. coke, or milk of any sort, are NOT permitted during this time.
Failure to adhere to these guidelines could result in your operation being delayed or cancelled.
Late morning/early afternoon admission for surgery that afternoon (eg.11:30 am or 1:00 pm admission)
You may have a light meal such as tea and toast BEFORE 7am but no food or milk after this time. You may drink water up until 11am. Please do not drink anything after this time.
Take any regular medication that has been prescribed by your GP and is due on the morning of your operation with a sip of water, unless advised by Pre-assessment Clinic staff.
Prescribed drinks for enhanced recovery should be taken in accordance with the guidelines given to you by the Pre-assessment Clinic staff.
Please do NOT chew gum, eat sweets or drink anything other than water. ALL other fluids, including tea, coffee, carbonated drinks eg. coke, or milk of any sort, are NOT permitted during this time.
Failure to adhere to these guidelines could result in your operation being delayed or cancelled.
What to expect
Before you come into hospital
You will be seen by a nurse in the Pre-Operative Assessment Clinic, who will check what medication you are prescribed and tell you if and when you need to discontinue any of your drugs before surgery. In most cases you will continue on all the drugs usually prescribed by your GP.
You should bring all your usual medication into hospital with you, which will be locked away in a medicine locker beside your bed. It is better to store and bring them in their original containers rather than to decant them or bring in single strips. This is so that we can check your dosage instructions and positively identify them as belonging to you.
Whilst you are in hospital
The doctor will prescribe on your drug chart your usual medication and any further drugs that you might need whilst in hospital. These usually consist of anti-sickness, painkillers and blood thinning medication. The pharmacist also checks your drug chart.
Discharge from hospital
Before discharge, the pharmacist will dispense an interim box of analgesics and any other medication prescribed by the doctor on your drug chart. If you need to continue with the prescribed treatment you will need to order more from your GP, before you run out.
Blood transfusion
Why might you need a blood transfusion? Most people cope well with losing a moderate amount of blood (e.g. two to three pints from a total of around eight to ten pints). This lost fluid can be replaced with a salt solution. Over the next few weeks your body will make new red blood cells to replace those lost. Medicines such as iron can also help compensate for blood loss. However, if larger amounts are lost, a blood transfusion is the best way of replacing the blood rapidly.
What might I do to reduce my need for blood before an operation?
- Eat a well-balanced diet in the weeks before your operation.
- Boost your iron levels – ask your GP or Consultant for advice, especially if you know that you have suffered from low iron levels in the past.
- If you are on Warfarin or Aspirin, stopping these drugs may reduce the amount of bleeding. You will be advised if you should stop these before your operation.
Are transfusions safe?
Almost always, yes. The main risk from a transfusion is being given blood of the wrong blood group. A smaller risk is catching an infection. To ensure you receive the right blood, the clinical staff make careful identification checks before any transfusion. They will ask you to state your full name and date of birth. They will then check the details on your wristband to ensure that you receive the right blood. They will regularly monitor you during your transfusion and ask how you feel.
Donated blood will be specially selected to match your own blood for the most important blood groups. But, because your red blood cells carry over 100 different blood groups, an exact match is not possible. About one in every 15-20 patients develops an antibody to the donated blood, and will need to have specially matched blood. If you have a card saying that you need to have special blood, please show it to your nurse. Fortunately, severe reactions to blood transfusions are extremely rare. But when they do occur, staff are trained to recognise and deal with them.
Please inform the orthopaedic team if your religion/belief system has an objection to you receiving blood products.
Other information
If you are interested in finding out more about blood transfusions and have access to the internet, you might find the following website useful:
National Blood Services – www.blood.co.uk
Anaesthesia and you
Anaesthesia and you
Preparing yourself for anaesthetic
- It is difficult to separate the risks of anaesthesia from the risks of the operation and your general health. The risks to you as an individual depend on whether you have any other illnesses and personal factors, such as whether you smoke or are overweight.
- If you smoke, giving up for several weeks before the operation reduces the risk of breathing problems and improves healing of the tissues. If you cannot stop, cutting down will help
- If you are very overweight, reducing your weight will reduce many of the risks of having an operation and anaesthetic
What will happen before my surgery?
You will meet your anaesthetist before your operation. They will ask you questions about your health, previous anaesthetics and usual medicines and will need to check your answers to other questions. They may need to examine your chest with a stethoscope and examine your neck and mouth. Please ask questions and tell them of any worries you may have.
You will receive clear instructions when to stop eating and drinking before your operation. It is very important to follow these or your operation may be delayed or cancelled.
It is important you continue to take all your usual medications, including inhalers, unless otherwise advised.
Types of anaesthesia
Spinal
Your surgery will usually be performed under a spinal anaesthetic. This is an injection of local anaesthetic into the back which causes numbness below the waist for several hours. During the operation, some patients may wish to be awake and listen to music, or watch a film. Others may wish to be more asleep either with light sedation or a general anaesthetic.
Spinal anaesthesia allows excellent pain relief in the immediate postoperative period. There is some evidence that it may improve or enhance the speed of your post-operative recovery. There is good evidence that it reduces the likelihood of post-operative confusion and delirium, particularly in older patients. There is strong evidence that it reduces the likelihood of post-operative nausea and vomiting.
As with all types of anaesthetic, spinal anaesthesia carries risk. Generally they are considered safe, as or safer than general anaesthetics. Many people often worry about back pain. There is no association between spinal anaesthesia and the development of back pain. Common side effects are related to the actions of the local anaesthetic on nerves and include low blood pressure, shivering and itching. These tend to resolve quickly after the spinal wears off (within a few hours).
Uncommonly (less than 1 in 200) some patients may get a headache afterwards. This will often be self-limiting, but may require further intervention. Nerve damage resulting in prolonged weakness or numbness is very rare (less than 1 in 10,000). Paralysis is extremely rare (less than one in a million). Your anaesthetist can discuss these risks with you if you are concerned.
General anaesthesia Nowadays general anaesthesia (GA) on its own is uncommon for hip or knee replacement surgery, as it does not provide any pain relief.
It is usually used in combination with a spinal anaesthetic or a nerve block. A GA consists of a combination of drugs, which are given to make you completely unconscious. During a general anaesthetic you do not feel anything and will not be aware of what is going on around you. When the operation is finished the anaesthetic is stopped and you regain consciousness.
Modern general anaesthesia is very safe. However, common side effects include a sore throat, feeling sick or vomiting, shivering or a headache.
Less common complications include chest infection, an existing medical problem getting worse, muscle pains, damage to the teeth, lips or eyes, and excessive drowsiness or slow breathing.
Serious complications related to general anaesthesia are rare but include: life threatening allergy to drugs, failure to maintain a clear airway and serious cardiac or respiratory complications, such as heart attack and stroke. Awareness or becoming conscious during your operation is also rare for this type of surgery. Nerve Block (Regional Anaesthesia) some patients may not be suitable for spinal anaesthesia for a variety of reasons. In this situation you may be offered a GA in combination with a nerve block. A nerve block is an injection of local anaesthetic near to the nerves that go to your leg. Most of the upper part of the leg will be numb and pain free usually for about 12 to 24 hours afterwards. You may not be able to move your leg properly during this time. The injection may be given before the general anaesthetic or when you are asleep. Due to the impact that this has on you mobilising on the day of and day after surgery, nerve blocks are being used less frequently.
Surgery
Your stay
Please have a bath or shower before your admission and please bring with you:
- Any drugs or inhalers you may take as prescribed by your GP
- Dressing gown and slippers (these are essential for your walk to theatre)
- Clothing that is comfortable and easy to put on for after your operation
- Toiletries
Please note: The time you have been instructed to arrive is an admission time and not the time of your operation. Your operation will be performed sometime during either the morning or afternoon.
Regardless of where you are admitted for your surgery, you may have to wait for your operation, so please bring something to keep you occupied. Yeovil Hospital has free Wi-Fi available on site.
General guidance for all surgical patients
On the day of your surgery please refrain from:
- Chewing gum or eating boiled sweets
- Driving yourself in or using public transport – please arrange for someone to bring you or get a taxi
- Bringing any jewellery or valuables with you. Please remove your wedding band before surgery
- Smoking
- Wearing make-up and nail varnish – please remove before arrival
- You may bring iPods/mp3 players (all we ask is that you try not to disturb other patients while using it). However, please do not bring other portable electrical equipment, such as a hair dryer
Please note: Yeovil District Hospital NHS Foundation Trust accepts no responsibility for the loss of, or damage to, personal property of any kind, including money. You are responsible for the safekeeping of your property at all times.
7:30am/8am admission - for surgery on the same morning
Do not eat anything AFTER midnight, or have milk, on the day of your operation.
You can drink water up until 6am and then nothing to drink after this time. Prescribed drinks for enhanced recovery should be taken in accordance with the guidelines given to you by the Preassessment Clinic staff.
Please do NOT chew gum, eat sweets or drink anything other than water. ALL other fluids, including tea, coffee, carbonated drinks eg. coke, or milk of any sort, are NOT permitted during this time.
Failure to adhere to these guidelines could result in your operation being delayed or cancelled.
Late morning/early afternoon admission for surgery that afternoon (eg.11:30 am or 1:00 pm admission)
You may have a light meal such as tea and toast BEFORE 7am but no food or milk after this time. You may drink water up until 11am. Please do not drink anything after this time.
Take any regular medication that has been prescribed by your GP and is due on the morning of your operation with a sip of water, unless advised by Pre-assessment Clinic staff.
Prescribed drinks for enhanced recovery should be taken in accordance with the guidelines given to you by the Pre-assessment Clinic staff.
Please do NOT chew gum, eat sweets or drink anything other than water. ALL other fluids, including tea, coffee, carbonated drinks eg. coke, or milk of any sort, are NOT permitted during this time.
Failure to adhere to these guidelines could result in your operation being delayed or cancelled.
Visiting
Visiting times vary and are limited on the wards to allow routines to be carried out and give patients sufficient time to rest. Please check visiting times with the Sister/Charge Nurse on the ward.
Meet the ward team
What to expect
Day 0 - Day of Arrival
You will be admitted either the day before or the day of surgery.
Please go to the ward at the time stated in your admission letter.
What to expect - immediately before surgery on arrival, you will have your blood pressure, temperature, pulse and oxygen saturation levels recorded.
- The anaesthetist and a member of the surgical team will visit you before surgery. The surgeon will discuss your consent again. The anaesthetist will review the anaesthetic and methods of pain control. You will have the opportunity to ask any further questions.
- A member of the surgical team will draw an arrow on your leg to ensure the correct side is operated on. Do not wash off this arrow!
- You will be given pre-operative painkillers. This is to ensure that they are in your bloodstream by the time of surgery.
- Theatres run all day, so your surgery could be in the afternoon.
- When it is time for your operation, you will be taken to the operating department holding area. There will be a series of patient checks that you go through to ensure your safety.
- You will then go to the anaesthetic room. Here you will meet your anaesthetist again, and there will also be an anaesthetic assistant.
- There will be a final series of checks and you will be attached to standard monitoring equipment.
- Anaesthesia will proceed as outlined previously.
During surgery, what does my anaesthetist do?
Whilst you are in theatre the anaesthetist will monitor vital signs to ensure that you are safe, and will also administer any drugs or fluids that may be necessary. Most patients will be having their surgery under spinal block.
If you are awake or under light sedation, you will be aware at times of some noises and vibrations. The anaesthetist will be there at all times to reassure you. You may wish to bring an iPod or tablet to either listen to music or watch a movie.
What to expect - immediately after surgery
The operation to replace your hip takes about 1 - 2 hours.
At the end of the surgery, the anaesthetist will take you to the recovery area for a short period of assessment. The drip in your arm should be removed once you are tolerating food and fluids. Your pain control will be established and your vital signs monitored. You will remain there under the care of a specially trained recovery nurse, until it is time for you to go to the orthopaedic ward.
Pain management
You should expect some discomfort following surgery. You will be given regular painkillers so you are able to do exercises and move your new hip. Please see the section on management of pain following surgery for further information.
Painkillers include paracetamol, ibuprofen-type drugs (non-steroidal anti-inflammatory drugs) and morphine-like drugs (opioids). Initially, you will need strong painkillers to help you to move. We will give you strong
Painkillers for one or two days after your surgery. Sometimes, these strong painkillers are given to you through a drip into your arm. Please remember to let the doctors and nurses know if your pain score is 2 (moderate) or above or if the pain stops you doing your exercises. We may need to alter or increase your painkillers.
Pain Score
How is pain assessed?
After your operation your pain will be assessed regularly, pain will be measured by using a pain score. You will be asked to describe your pain on a scale of 0 - 10. Zero being no pain and ten being severe pain.
Pain Score
How would you describe your pain?
- No pain at all
- Pain
- Increasing
- Hurts on movement
- Moderate pain All the time
- Severe pain all the time
- Worst pain ever
- Had Dull ache
- Mild pain all the time
Some patients experience side effects from painkilling drugs.
These can include:
- Drowsiness (feeling sleepy)
- Nausea or sickness
- Indigestion (heartburn)
- Constipation
If you have any concerns about your pain or the painkillers that you are given, you may discuss this with your nurse or doctor. You can also be referred to the Pain Specialist nurses if your pain is difficult to manage.
Day 1-3
Day one - after surgery
- You will be assisted to wash and you will get dressed.
- You must not attempt to get out of bed until you have been assessed you will be helped out of bed and sat in a chair.
- If you are drinking sufficiently your drip will be discontinued.
- The dressing on your wound will be checked daily.
- You will be seen by a member of the medical team.
- Your pain levels will be assessed and pain relief will be given as appropriate.
- You will be given regular pain relief medication by mouth.
- Many of these medications make you constipated and you may need laxatives to counteract this.
- Throughout your stay please let the nurses know if you have not had your bowels open so they can address the problem.
- The Physiotherapist will see you and start your exercise regime.
- On day one or two, bloods tests will be taken and you may need a blood transfusion or to commence iron tablets.
- Your drain and urinary catheter, if you have one, may also be removed.
Day two
- You will be assisted to sit in a chair for your breakfast and your wash.
- You will be asked to get dressed.
- From now on you will be expected to sit in a chair for all meals.
- The physiotherapist will continue with your exercises and progress your mobility with a walking aid.
- You will be taught to go up and down stairs if you are ready.
- You will be assisted to walk to the toilet and if possible back again.
- If you have not been seen by the occupational therapist (OT) before your operation an initial assessment will be made today.
Day three
- The physiotherapist will continue with your exercises and progress your mobility with a walking aid. They will also check that you are familiar and comfortable with your exercise regime.
- You will be taught to go up and down the stairs if you have not already done so.
- You will be encouraged to walk to the bathroom for your wash. The nurses will assist you as required.
- The OT will see you to confirm your discharge arrangements and issue any required equipment.
- The OT will ensure that you can transfer on and off the bed, chair and toilet unassisted before you go home.
- You will be ready to go home as soon as you have met your discharge goals.
Preparing to go home
After your operation
Once you have sufficiently recovered from your anaesthetic, and you have met the criteria for safe discharge from theatres, the Theatre Recovery team will escort you to the ward. They will hand your care over to the ward nursing team who will continue to monitor your progress by:
- Frequently observing your pulse, blood pressure and temperature
- Monitoring and assisting you in managing any pain you may have
- Checking your dressing (and drain if you have one)
- Assisting you to turn and move to get comfortable
- Do ask for help in getting up the first few times – you may not feel very steady
- You will be asked to do deep breathing and coughing exercises and to move your legs
The following document contains lots of useful post-operative advice.https://yeovilhospital.co.uk/wp-content/uploads/2021/08/THR-Presentation.pdf
Discharge
Important Contact Information
Yeovil District Hospital 01935 475122
Ward 6A (Elective surgery ward) 01935 384322
Orthopaedic Outpatients 01935 384319
Pre Assessment Clinic 01935 384863
Joint Replacement Clinic for Hips 01935 606099 Occupational Therapy and Physiotherapy
Wound care
Please see the following information on Discharge after your hip replacement.https://yeovilhospital.co.uk/wp-content/uploads/2021/08/Discharge-home-after-your-knee-replacement-Feb-2021-002.pdf
Physiotherapy
Please see the attached document outlining the exercises you should undertake when recovering after your hip replacement. https://yeovilhospital.co.uk/wp-content/uploads/2021/08/Hip-Excercise-Pics-1.pdf
Your Follow Up
Placeholder…
Frequently Asked Question
Which ward will I be admitted to?
6A is our elective orthopaedic ward however, it may be that you stay on a different ward during your stay. This will always be confirmed with you and you can be reassured that all your needs will continue to be met.
What time should I arrive on the ward?
Generally you will be asked to come in for 7am on the morning of your surgery however, in some circumstances this may change. You will be told in advance what time you should arrive.
Why is my leg marked prior to surgery?
Your consultant may perform multiple operations each day and the washable arrow is merely confirmation that they are operating on the correct leg.
How long will my operation last?
Times vary but on average your operation will last approximately two hours.
Should I bring my own painkillers to hospital?
You should not bring your own medications in to the hospital but do inform the medical staff of any regular medications that you do take.
Does positional advice mean I have free movement and can return to normal physical movement as soon as pain allows?
While positional advice does afford you more freedom of movement after your operation, you should always be cautious when bending, twisting and crossing your legs. If you do attempt to bend down to your feet, movement should be slow and you should avoid twisting. Crossing the legs is not good for circulation anyway so this should be avoided. These particular movements should not be done to the excess.
Which side of the bed should I get in/out from?
It is advisable to lead out of bed with the operated leg and lead in to bed with non-operated leg. This is for your comfort and to reduce the risk of your new hip being put in an awkward position. You should always listen to your body and you shouldn’t ignore discomfort.
Why might I not be able to get out of bed the day after surgery?
Early mobilisation is strongly encouraged however, low blood pressure; low oxygen levels and dizziness/nausea can often restrict patients the first day after surgery.
Will I be given a walking aid to go home with?
You will be provided with either a pair of sticks or a pair of crutches for discharge. In rare circumstances, you may also be provided with a wheeled walking frame.
I don’t have stairs at home but is it worth practising them anyway?
Have a think about properties you may be visiting in the coming months; are there stairs? If so, it’s worth having a practise under supervision.
When will I be allowed to walk alone on the ward?
Once the physiotherapy team are happy that you are safe mobilising alone and at very low risk of falling, you will be encouraged to mobilise as often as possible and without direct supervision.
When should I start doing the exercises and how long for?
It is advisable to begin exercising in the weeks leading up to your operation and to continue with them for several months after surgery. Exercises will strengthen the muscles around your hip joint and give you the best possible outcome.
I have my own crutches/sticks, can I bring these with me?
Yes, if you have a pair that you find comfortable to use. We will always check that your aids are suitable to be used first and may provide new aids if yours is not fit for purpose.
Please label any mobility or dressing aids that you bring in to the hospital.
Do I keep all equipment that is provided by the hospital?
Mobility aids and raised equipment are provided to you on a temporary loan basis only and they should be returned once they are no longer required.
My partner had a hip replacement and needed all furniture to be raised; why is it not essential that furniture is raised for me?
Furniture heights are assessed on an individual basis based on the patients’ lower leg measurement. Therefore if you are shorter than your partner, this will likely be the reason why furniture does not need to be raised for you.
Can I use the bath after my operation?
It is not advisable to sit in a bath for three months after your hip replacement. However, if you are asked to follow positional advice then you will be able to get in to a bath and shower in standing. It is advisable to sit on the edge of the bath and lift your legs over the side.
How soon can I use the shower after my operation?
Your wound dressing is water resistant therefore you are allowed to use the shower as soon as you feel physically able to do so. You shouldn’t, however directly soak the wound area.
Can you provide me with a shower stool?
Unfortunately, we are unable to issue shower stools. They can however, be purchased from many high street and online retailers.
It is important to note that perching stools should not be used in a shower.
What is the most comfortable way to lower myself down in to sitting?
It is recommended that you use an armchair for at least the first few weeks after your surgery as you then benefit from having solid arms both sides. It is also advisable to step your operated leg out in front slightly as you lower to take pressure off of the hip.
My only toilet is upstairs, is this an issue?
Not necessarily as you will be shown how to manage the stairs during your admission. If you have concerns about getting to the toilet in time or have a condition that means you experience frequency/urgency, discuss this with the occupational therapy team as they may be able to supply a commode for downstairs use (subject to criteria).
I have no immediate family; who can help me with shopping and housework?
You should plan for this prior to admission to hospital and ensure that your home is well stocked with food. Certain charities and voluntary organisations may be able to support with food shopping and you should contact them directly to discuss your needs.
Generally, these types of organisations do not offer support with housework therefore you should seek private help. See the Useful Contacts sheet for further information.
Will I be able to carry things?
You should not carry items while you are using mobility aids as this increases the risk of losing your balance.
Further advice regarding transporting meals etc. can be given by the occupational therapy team and helpful aids such as a kitchen trolley may be supplied if required (subject to criteria).
How do I reach down to my feet after surgery?
Dressing aids are extremely beneficial after hip surgery. They enable individuals to maintain their independence whilst avoiding uncomfortable bending/twisting.
When can I return to driving?
You should not drive for six weeks after hip replacement surgery. After this time, you should be cautious and only return to driving if you are confident that your pain is well controlled and you could perform an emergency stop if required.
I drive an automatic car, can I drive straight away?
This will depend on which leg has been operated on and your consultant’s advice.
Will transport be provided to take me home?
Hospital transport will not be provided (unless under exceptional circumstances) and you should arrange for a friend or family member to collect you from hospital. Voluntary services and taxis should also be considered to assist with transport.
What things might delay my discharge?
The most common reasons for a delayed discharge are:
Leaking wound site
Low blood pressure
Awaiting post-operative x-ray
Equipment
Whilst medical reasons are beyond anybody’s control, please help avoid equipment delays by providing your furniture heights when they are requested.
Do you provide respite stays?
Yeovil Hospital does not fund or arrange respite stays following an admission. If you have concerns about returning straight home after surgery then you should make arrangements for this prior to admission.
Will I receive regular physiotherapy after my surgery?
We do not provide routine rehabilitation following surgery unless there is a clinical need (assessed on an individual basis).
You should continue completing your exercises once home and aim to increase your walking distance every day.
You will be provided with a follow up appointment to take place approximately three weeks after surgery.
What does my follow up appointment involve and how long does the appointment last?
You will have a wound check; exercises will be reviewed and progressed if needed; your gait pattern will be assessed and stairs may also be reviewed. You will have the opportunity to ask any questions and it will be determined whether further physiotherapy follow up is required.
The appointment lasts approximately twenty minutes and generally you are discharged at this time to continue with your rehabilitation at home.
Ref: 01-21-34
Review: 08/23








