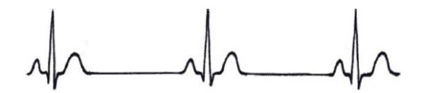
Normal Heart Rhythm
A normal adult heart rhythm is regular and usually beats around 60 to 100 beats per minute at rest. The heart has its own natural pacemaker called the sinus node, which sends out regular electrical impulses that travel through the heart’s conduction system. This causes the heart muscle to contract and pump blood around the body.
Why do I need a pacemaker?
Problems with the heart’s own conduction system can result in your heart beating too slowly. This can cause some patients to feel unwell and have symptoms such as dizziness, syncope/collapse and extreme tiredness.
The following conditions may require you to have a pacemaker fitted:
- Sick sinus syndrome: The heart’s natural pacemaker (sinus node) does not function properly causing the heart to beat too slowly or too fast.
A pacemaker will correct the slow heart rate and medication can be used to help prevent faster heart rhythms. - Heart block: Conduction problem resulting in failure to transmit electrical impulses from the top chambers of the heart (atria) to the bottom of the heart (ventricles).
- Atrial Fibrillation: An irregular heart rhythm
originating from the top chambers of the heart (atria). This can be too fast or too slow, or a combination of both.
A pacemaker may be implanted to prevent your heart from beating too slowly. The pacemaker cannot stop your own heart from beating too fast. Abnormal faster heart rhythms are treated and controlled with the use of medication.
How does the pacemaker work?
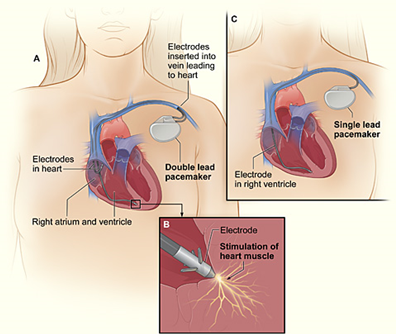
A pacemaker consists of a pulse generator (pacemaker box), which sits under the skin in the upper chest, and either one or two electrode leads that sit inside the heart. The pacemaker box contains the power supply (battery), electronic circuit and specialised software and memory in order to monitor your heart rhythm and rate. The electrode lead(s) are thin, insulated wires that deliver electrical impulses from the pacemaker box to the heart. Each electrical impulse sent from the pacemaker travels down the lead to stimulate the heart to contract and produce a heartbeat.
Your pacemaker may not have to work all of the time, depending on how fast your own heart rhythm is. Most pacemakers are set to work “on demand”. The pacemaker will constantly monitor your own heart’s rhythm and will only work when your heart rate goes too slow. There are many different pacemaker settings and these will be optimised to suit you during pacemaker follow up appointments. There are many different pacemakers and pacemaker manufacturers. Physicians and pacemaker technicians will select the most appropriate pacemaker for you.

There are two types of pacemakers to correct slow heart rhythms, these are:
- Single chamber pacemaker (one electrode lead)
- Dual chamber pacemaker (two electrode leads)
The pacemaker generator/box is contained within a protective metal casing (usually titanium).
Most pacemakers are powered by a lithium battery. Battery life can vary depending on different factors, such as what type of pacemaker you have and how much the pacemaker is being used, but can usually last between 6 and 10 years. The batteries are not rechargeable and once the battery has depleted, the pacemaker box will need to be replaced.
How the pacemaker is fitted
On the day of the procedure you will be seen in the Cardiac Rehab Department by one of the cardiac nurses who will get you ready for your procedure. You will need a cannula inserted into your arm and you will be given a one off dose of antibiotics. Once you are ready, you will be taken round to the Radiology Department where your procedure will take place.
A doctor, nurse, pacing technician and radiographer will be present during the procedure. You will be asked to lie on a narrow operating table. The procedure is carried out with just the use of local anaesthetic. Sometimes very mild sedation can be given, if you feel that you need it. This will make you feel relaxed and sleepy.
The skin where the pacemaker will be implanted will be cleaned with antiseptic solution and local anaesthetic injected under the skin.
The doctor will make a small incision where the pacemaker will be inserted and also locate the vein in which the electrode lead(s) will be passed through to the heart. The leads are inserted into the vein and guided to the correct position within the heart using x-ray screening. Just before the lead(s) are connected to the pacemaker box, a pacemaker technician will test them to ensure they sense your own heart’s electrical signals and stimulate the heart appropriately.
During the procedure you may feel a bit uncomfortable and may feel some pushing and pulling sensations. You may feel your heart beating faster, some fluttering or palpitations might be felt, whilst the leads are being guided into place and checked.
You may also be asked to take some deep breaths in and give a cough during the checking procedures. The pacemaker box will be implanted under the skin in either the left or right side of your chest (depending on whether you are left or right handed).
Although pacemakers are now relatively small, they can sometimes still be seen underneath the skin. The incision site will then be stitched with dissolvable stitches and covered with a protective dressing. A pressure dressing may also be applied.
Changing the battery
This is a similar procedure to the original pacemaker implant except the pacemaker leads will not be changed, just the box.
Are there any risks associated with the procedure?
There is a small risk of infection, bleeding and bruising to the pacemaker site. There are some other small risks associated with having a pacemaker fitted that your doctor/nurse will discuss with you in detail before you sign your consent form for the procedure.
After having the pacemaker fitted
Following the pacemaker implant you will be monitored for a few hours and have a chest x-ray. You will then be sent home as long as you have someone at home with you overnight. If there are any problems during the procedure, you may require an overnight stay. You may feel some pain or discomfort and there may be some bruising around the pacemaker site. You will be able to eat and drink immediately after the procedure. You will need to return to the hospital the next day and the pacemaker will be checked.
Most people have no problems after having a pacemaker fitted, but if you experience dizziness, breathlessness or symptoms similar to those that you may have felt prior to pacemaker implant such as syncope/collapse, you should contact your GP or pacemaker clinic.
You will be given a pacemaker identification card before leaving hospital. This will have details of the make and model of your pacemaker. It is useful to ALWAYS carry this card with you in case of an emergency.
Contact information
Clinical Investigations Department
- Technicians: 01935 384 610
- Appointments: 01935 384 457
Cardiac Rehab Department
- Specialist Nurses: 01935 384 884
Ref: 02-20-102
Review: 02/22








