Please read this information as soon as you receive your appointment date and time. 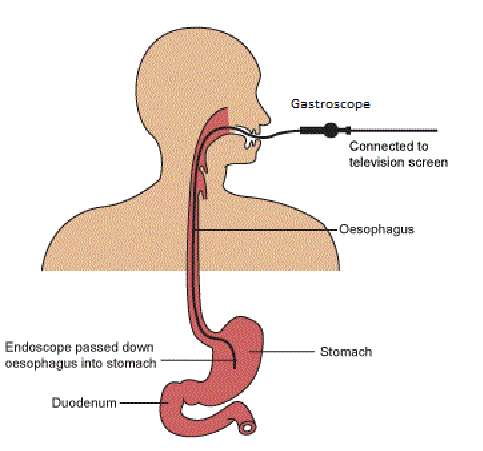
This information has been written to enable you to make an informed decision when you are asked to give
consent to the procedure. If you find you have any questions or concerns, please contact the Day Surgery Unit on 01935 384 339, or you can speak to the nurse or endoscopist when you arrive.
A gastroscopy involves passing a small scope (tube) over your tongue, down your throat and into your stomach. This is a flexible tube with a light and a camera in its tip. When air is put into the stomach, the doctor can examine the lining and take small samples (biopsies).
Essential guidance before procedure
- If your appointment is in the morning, it is essential that you have NOTHING to eat from midnight the night before your appointment.
- If your appointment is after 1pm, have a light breakfast, eg. cereal or toast before 7am and NOTHING to eat after that.
Please do not wear any type of false nails or nail varnish, as it interferes with our staff monitoring your vital signs throughout the procedure.
You may drink clear fluids up to four hours before your appointment time.
For your own safety it is important that your stomach is empty at the time of examination. Any food or drink taken within this time will stimulate your stomach to make acid which could damage your lungs if inhaled during the examination.
Please Note: If you are taking medication to stop your blood clotting e.g. warfarin, clopidogrel, dabigatran, please contact us as soon as you receive your appointment.
If you are a diabetic on medication, please follow the following information. If you are unsure what to do please contact the diabetic sisters on 01935 384 517 for advice before your admission. Please be aware that the instructions for morning and afternoon are different.
Morning procedure
You must have nothing to eat or drink from midnight.
If your diabetes is controlled by diet alone:
Follow the usual instructions in the Day Surgery information booklet you will have been given.
If you take tablets for your diabetes:
- On the evening before the procedure, make sure you have an extra snack before going to bed
- On the morning of your procedure do not take any food, drink or tablets for diabetes
- If you monitor your blood glucose, check it before coming into hospital. If it is below 4mmols/litre follow the instructions for hypoglycaemia (see opposite page)
- Bring all your medication in with you
- The Day Surgery staff will monitor your blood glucose level
- After the procedure you will be given food and drink. You may take your usual tablets for diabetes then
If you take insulin for your diabetes:
Please note: If your insulin is called Lantus (Insulin Glargine) or Levemir (Insulin Detemir) continue to take your normal dose.
- On the evening before the procedure, make sure you have a snack before going to bed. After midnight you may have nothing to eat or drink. In the event of hypoglycaemia, see below.
- On the morning of the procedure, do not take any insulin or diabetes tablets
- Check your blood glucose before coming into hospital and follow hypoglycaemia instructions (see opposite page) if below 4 mmol/litre
- Bring all your insulin and medication with you
- The Day Surgery staff will monitor your blood glucose level
- After the procedure, you will be given food and drink. Take your normal morning dose of insulin now and eat normally for the rest of the day
Afternoon procedure
If your diabetes is controlled by diet alone: Follow the usual instructions in the Day Surgery information booklet you will have been given.
If you take tablets for your diabetes:
- On the morning of the procedure
- do not take any tablets for diabetes
- Have a light breakfast before 7am (eg. cereal or toast), do not eat anything after this
- You may drink clear fluids (no milk) for up to four hours before your appointment
- If you monitor your blood glucose, check it before coming into hospital. If it is below 4 mmols/litre, follow the instructions for hypoglycaemia (see opposite page)
- Bring all your medication in with you
- The Day Surgery staff will monitor your blood glucose level
- After the procedure you will be given food and drink. You may take your usual tablets for diabetes then
- If you take diabetic tablets twice a day, only take the evening dose
If you take insulin for your diabetes:
Please note: If your insulin is called Lantus (Insulin Glargine) or Levemir (Insulin Detemir) continue to take your normal dose
- Give ½ your usual dose of insulin with your usual breakfast before 7am. Do not eat anything after this
- You may have clear fluids (no milk) for up to four hours before your appointment
- Check your blood glucose two-hourly before coming into hospital and follow hypoglycaemia instructions if below 4 mmol/litre (see opposite page)
- At 12pm, take glucose to reduce the risk of hypoglycaemia (see hypoglycaemia information below)
- Bring all your insulin and medication with you
- The Day Surgery staff will monitor your blood glucose level
- After the procedure, you will be given food and drink
- Take your normal evening dose of insulin prior to your evening meal
Treatment for Hypoglycaemia (if blood sugar less than 4 mmol/litre)
- Take four glucose tablets
- Repeat blood sugar test after ten minutes
- If still below 4mmol/litre repeat the above
- Check your blood sugar hourly
- On arrival at the Day Surgery unit, you must inform the nursing staff of this episode.
If you take medication for your stomach, please stop taking these one week before your appointment, unless you have been specifically asked to continue (for example patients with Barretts Oesophagus). This includes: Omeprazole (Losec, Mepradec) Pantoprazol (Protium) Rabeprazole (Pariet) Lansoprazole (Zoton) Esomeprazole (Nexium, Emozul) Cimetidine (Tagamet) Famotidine (Pepcid) Nizatidine (Axid) Rantidine (Zantec) If you are taking medication to stop your blood clotting eg. warfarin, clopidogrel, dabigatran, please contact us as soon as you receive your appointment.
Other medication
All other medication should be taken as prescribed. Small sips of water can be taken with medication only. If you are having chemotherapy please inform us on receipt of this letter. You will be informed by the endoscopist on the day of your procedure when to restart any medication you have stopped. Please ask any questions you have if you are unsure.
What to bring with you
You may want to bring a book or something to read, you should expect to spend up to two hours with us but delays do occur so this can occasionally be longer. Remember, your appointment time is not the time of your examination, we also look after emergencies and these take priority on our lists. You do not have to change your clothes so nothing else is required but please leave any valuables at home.
What happens when you arrive
Your details will be taken and checked by our receptionist. You will be shown to our lounge or a cubicle and a nurse will take your blood pressure and ask you some questions about your health.
Consent
A doctor or nurse will come and explain the examination and answer any questions you may have. We do have a small number of trainee endoscopists in the department, who work under direct supervision from an experienced endoscopist.
Risks
Complications, although rare, can occur with this procedure. These include:
- There is a small risk to teeth/dental work if they are already damaged or loose
- A sore throat or bloated feeling is not uncommon
Other complications are more rare (less than one in 1,000) and include:
- A perforation or tear of the gut wall (this could require an operation to repair)
- Bleeding
- An allergic reaction to the medication
- Infection
The endoscopist will speak to you before the procedure, so please feel free to ask any questions.
The examination
A gastroscopy can be performed either with a local anaesthetic throat spray or light sedation. The choice is yours, but the following should be considered: Throat spray: This will numb the back of your throat making it more comfortable to swallow the tube. The throat spray will wear off completely within an hour and you will be able to eat and drink with no further effects. Intravenous sedation: This will be given via a needle in your hand or arm. The sedation will relax you and may make you drowsy but will not put you to sleep. You will hear what is said to you and be able to respond to any instructions given to you. The sedation will affect your judgement, memory and reflexes for up to 24 hours. As with any other medication, there is a small risk of an adverse reaction to the sedation. A nurse will attach monitors for recording your pulse, oxygen levels and blood pressure throughout the examination if you have intravenous sedation. You will be asked to lie on your left side and a mouth-guard will be placed in your mouth to enable the scope to pass through. A nurse will remain with you to reassure you, to suck out any secretions from your mouth, and tell you what you need to do and what to expect.
After the procedure
If you have a throat spray: You are able to leave after checking with the ward nurse for any further instructions. You must wait about 30-40 minutes before having a drink to make sure the effects of the throat spray have gone - always start with water. If you have sedation: You will have to stay with us for up to two hours after the procedure. You MUST be accompanied home and have some one stay with you for the first 12 hours. The effects of the sedative can last up to 24 hours so you should not drive, operate machinery or drink alcohol during that time. We advise that you arrange alternative care for young children or elderly relatives for 24 hours after having sedation. The endoscopist will inform you of the test results on the day of your examination but if any samples have been taken, these results may not be available for one to two weeks. It is important that you recognise the early signs of complications and contact your doctor if you have severe pain, difficulty in swallowing, vomiting, fever, chills or black stools. If a follow up appointment is necessary, it will be sent to you.
When can I eat and drink?
If you have had throat spray for your procedure, it will take 30 minutes for your swallowing to return to normal. After this time you may have a cool drink - you are at risk of burning yourself with a hot drink. You may eat and drink normally after this time. Your throat may feel a bit sore. If you have had sedation, you may eat and drink when you feel safe to do so.
When can I go back to work?
This depends whether you have had sedation or throat spray during your procedure. We advise that you refrain from work for 24 hours if you have had sedation. You must not operate machinery and your car insurance will not cover you to drive during this time. If you have had throat spray you may return to work when you feel safe to do so.
Will I be told any results after the procedure?
The endoscopist will speak to you after the procedure and explain any results to you. We will discuss the follow-up plan of care. We will give you a copy of your endoscopy report and a patient care report to explain any findings and give you advice for the next 24 hours.
Important contact numbers:
Endoscopy admissions office 01935 384793 Day Surgery Unit – between 8am and 7pm 01935 384339 After 7pm, call the Clinical Site Manager 01935 384 525
Protection your privacy and dignity
In order to preserve patients’ privacy and dignity, and to comply with Department of Health standards, the Endoscopy / Day Surgery Unit is unable to accommodate the relatives and friends of patients attending the department. Please leave a telephone number for your named contact and a member of the team will ring them when you are ready to leave the department. If they wish to wait for you in the hospital building, there are two coffee shops on Level 3 (Ground Floor) and “The Canteen” restaurant is located on Level 2. In certain circumstances, exceptions may be made if considered to be in the patient’s best interests. Please contact the Unit Sister on 01935 384 339 if you require further advice. Thank you for your cooperation. 








