This information is written to guide you and your relative/carer through your hospital stay.
Our aim is for you to regain a good level of mobility and be able to return to your home environment as soon as possible
with an appropriate level of assistance.
After your injury, you may have a number of questions about what has happened and how you will be treated. The following information aims to answer some of these questions. Should you require further details, do not hesitate to speak to staff involved in your care.
What is a hip fracture?
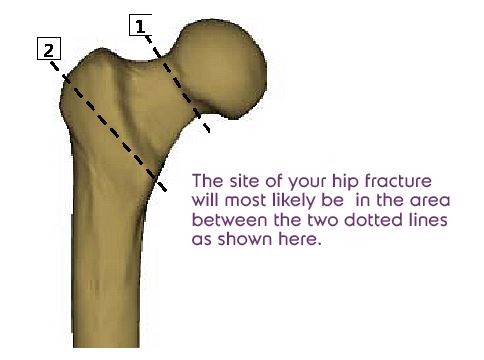
The bone you have broken is the femur (thighbone). The fracture will be between one and five inches from the hip joint. Fractures can be very different - from a simple crack to a complete break in which there are many fragments. The exact method of treatment will therefore depend on the type of fracture and where it is sited.
On arrival at the hospital
Your care will begin in the Emergency Department
- A doctor will see you and will request an xray of your pelvis and chest. An examination will be performed and a medical history taken. It will be important to know the details of your fall such as what caused you to fall and if this was the first time it had happened
- You will be asked if you have any allergies
- You will be given pain relief, usually as an injection
- A small plastic tube will be placed into a vein to enable you to have fluids or medication by drip as required
- Blood tests will be taken. Occasionally other heart investigations may be requested, these will be carried out prior to your surgery
On arrival to the ward
Once you arrive on the ward, you will be introduced to members of the staff that will be looking after you.
The doctor will explain about your operation. There are different ways of giving you an anaesthetic and these will be discussed with you.
At this stage, you will need to remain in bed on a special air mattress to help prevent your skin getting sore. You may be able to use bedpans/bottles to pass urine or it may be necessary for a urinary catheter (small tube) to be inserted into your bladder to enable you to pass water. You will need to use a bedpan for opening your bowels.
We will aim to preform your operation in the first one to two days of your admission wherever possible, unless you need other treatment first.
- You should not eat or drink anything, for at least six hours before your surgery (unless otherwise directed)
- You will be helped to wash and be given a theatre gown to wear
- You will have an arrow drawn on your injured leg and you will see the senior surgeon who will be performing your operation
- A member of the surgical team will go through the consent forms with you before your operation
- You will be taken to theatre on your bed
- There may be trainee clinical staff present in the operating theatre to observe the hip repair procedure as part of their training. If you have any objections to this, please inform us as soon as possible
This may vary from person to person
- You will wake up in the recovery room
Your pulse, blood pressure, temperature and hip wound will be checked frequently - You may have continuous fluids given through your drip
- You may be given oxygen by way of a mask or through little plastic tubes placed under your nose
- You may have a pillow or a foam wedge under or between your operated leg. This is to keep your leg in the correct position and you will have calf pumps to reduce the chance of blood clots forming in your legs
- You may have a daily injection under the skin which also reduces the chance of clots forming
- You may have a urinary catheter in place
- Your operation site can be closed using clips or soluble sutures. Clips usually are removed 12-14 days post surgery if you have been discharged from hospital the practice nurse at your GP practice can remove them, otherwise the ward staff will take them out. However, sutures need the ends trimming around 12 days after your surgery and should dissolve over a period of three to six months
Eating and drinking
As soon as you are able, you will be encouraged to start eating and drinking. You may also be encouraged to have supplement drinks in between meals to help build up your strength.
The treatment for the majority of hip fractures is an operation to repair the break, as without surgery many people will be unable to walk again. Most patients are treated with one of five types of hip repair.
Hemiarthroplasty
 This is a procedure which involves taking out the broken piece of bone and replacing it with an artificial hip joint (see picture below). It is used for those fractures which occur near the hip joint (position 1 on the hip joint diagram). The hip joint is a ball and socket but for Hemiarthroplasty only the ball part of the joint is replaced. The socket is not damaged and is therefore left intact.
This is a procedure which involves taking out the broken piece of bone and replacing it with an artificial hip joint (see picture below). It is used for those fractures which occur near the hip joint (position 1 on the hip joint diagram). The hip joint is a ball and socket but for Hemiarthroplasty only the ball part of the joint is replaced. The socket is not damaged and is therefore left intact.
Multiple screws

Three stainless steel screws are used to hold the bones in place for fractures near the hip (position 1). The operation to put in these screws is much smaller than that for a new hip joint. The operation is done through a small cut on the leg using x-rays to guide the position of screws and therefore, there is a reduced risk of infection or of problems with the wound healing.
Dynamic hip screw

This is a stainless steel plate, which is placed across the fracture and held in place by a number of screws. It holds the bones in position whilst they knit back together. It is only used for those fractures that are further away from the hip joint (position 2).
Intramedullary nail

This is a metal rod, which is passed down the cavity in the centre of the bone with additional cross screws to go across the fracture. It is only used for fractures that are in position 2 orfurther down the femur bone.
Total hip replacement
The hip joint is made up of a ‘ball’ and ‘socket’. During a total hip replacement the ‘ball’ (head of the femur) and the ‘cup’ (the socket in the pelvis) are replaced by artificial parts.

Pain control
You will be given regular medication to control your pain. However if you find that you are still in pain and it stops you moving around or sleeping, please do tell a member of staff.
Medical review
You will be seen by a senior doctor from the elderly care team and /or the specialist nurse for hip fractures this may not be until after your operation. They will look at how you can reduce the risk of falling again and/or breaking another bone.
This can involve you being referred for further investigation with the fracture liaison service, or you being prescribed osteoporosis medication. However, this will be discussed with you/relative/carer.
Some patients can suffer from a condition called delirium: This can be an upsetting situation for all concerned. If you have any concerns about a cognition or behavior change in your friend/relative please alert the ward staff. (There are leaflets available to explain the condition and coping mechanisms).
The specialist nurse for hip fractures will make contact with you about three to four months after your hip fracture. This can sometimes be in the form of a telephone call to your home address or a simple questionnaire. You will be asked questions to see how you are progressing after your fracture.
Planning your discharge home
Healthcare professionals will gather relevant information identifying your needs so that a plan for your discharge is started. Personal details and home circumstances will be discussed, ie. who lives with you; do you have stairs or do you have any community help which will need to be cancelled whilst you are in hospital. This information is important for your discharge planning and with the correct information, we may get you home faster. We may refer you to the Health and Social Care Team to look at potential help you may need when you leave hospital.
The following timetable is intended as a general guide after your surgery but individual patients will vary:
- You or your carer should arrange for day clothes to be brought into hospital
- You will have a blood test
- Your drip will be taken down once you are drinking
- Normal diet and fluids will be resumed. You can eat normal meals
- Your bladder and bowel functions will be monitored and any difficulties addressed
- You will do ankle and breathing exercises
- You will be taught exercises to strengthen your hip by the therapist
- You will be assisted in sitting on the edge of the bed. If you are able, you will be assisted to sit out in a chair
- You may start to take a few steps with assistance from staff
- Your therapist will ask a few questions about home
- If you live in your own home, your therapist may issue you with a furniture heights form. This is for a friend or relative to complete about details of your furniture heights
- The therapist will ask you or your carer details about your home environment/social situation and how you managed your day to day activities before your hip fracture
- If there are particular hip movements you need to be careful about, your therapist will discuss this with you or your carer and give written information
- You should continue to do the exercises you have been taught. You may also be given some additional exercises
- You should continue to do the exercises you have been taught. You may also be given some additional exercises by the therapist to do whilst standing
- You will be encouraged to dress in your day clothes Assistance from staff is available if needed
- Your bladder and bowel functions will continue to be monitored. If you have a catheter inserted, this will be removed once your bowel function has returned
- You will continue to practice your walking with assistance and/or supervision as required. The aim is for you to walk a little further each day in preparation for your discharge
- As your mobility progresses, the therapist will assess whether there are aids you may need at home and help arrange this
- The therapist will look at ways in which you can manage your day to day tasks if you come from your own home
- If you require additional assistance at home, our team will make the necessary referrals to assist this process
- If you need to climb stairs at home you will practise this in hospital with the therapist
- Some individuals may need to consider having a bed brought downstairs, this will be discussed with you by your therapist
- You will need to think about how you will get home. Please discuss transport arrangements with the nursing staff
- Before you are discharged, the ward staff will arrange your medication and discharge letters to take home
Getting mobile once you are home
You will probably find getting in/out of bed difficult to
begin with. You might need help at first to lift your leg across the bed until your strength returns. Your early therapy exercises will help you with this.
To get into bed:
- Back up to the bed, then sit down in the way you have been taught, supporting yourself on the bed, with the operated leg straight out in front.
- Move back across the bed and up towards the pillows, using your arms and un-operated leg to support you as you lift your bottom. Keep your operated leg straight, and both head and body in line. You can bend your un-operated leg.
Getting out of bed:
If possible lead with the operated leg. (If you are unable to do this at home, please speak to the therapist who will be able to advise you.)
- Use your arms and good leg as before, to slide yourself across to the edge of the bed.
- Slowly lift your bottom around, keeping your head and legs in line, until both legs come forward off the bed and down to the floor.
- Keeping the operated leg out in front, stand up in the way that you have been taught.
When sitting down or standing up from a chair, remember to hold onto the arms as you raise/lower yourself. When sitting, put the operated leg out in front of you, but try and limit this habit as you improve in your rehab.
Your chair or toilet may need to be raised or you may need rails to assist you. Your therapist will gather this information from your relatives and discuss your needs for discharge. Do not pull up on your walking aid.
If you normally dress independently, your therapist will discuss personal care with you. They may suggest long-handled aids to assist you when dressing.
- Sit on the bed or chair
- Take your time
- Dress your un-operated leg first and undress it last. It is likely to be easier for certain garments.
- Always wear flat, supportive, well-fitting footwear and, where possible, no laces
- Do not twist around to pick things up from behind you
If you are normally independent in kitchen tasks you may find the following points helpful. Your therapist will look at your individual needs:
Consider sitting to do activities (use a high stool)
Bring frequently used items to worktop height
Do not carry items whilst using your walking aid. Move them within arms’ reach along your worktop or other surfaces
If you live alone or have no one to carry meals/drinks for you, you will need to eat/drink in the kitchen. You may find a high stool helpful. You may need to find an alternative way of carrying items from the worktop to the table. Your therapist will discuss this with you and identify any aids required
Reaching low surfaces / items
Use a long-handled reacher, or grip a firm support, eg, a table; put your operated leg straight out behind you and bend the un-operated leg at the knee – using your arm for support.
Stairs
Take one step at a time
A therapist will show you the correct way of going up and down stairs and you will have a chance to practice them if needed
Going upstairs
Lead with your un-operated leg, the stick follows last
Going downstairs
Lead with your operated leg, the stick goes down first
- You should avoid cars with low seat heights, eg. sports cars or old style minis
- Ensure that you are standing on road level and not on a raised kerb so that you have extra seat height
- You should sit in the front passenger seat. The seat should be pushed back as far as it will go and partly reclined before you sit down, the driver should do this for you if the handles and/or buttons are low
- Turn with your back to the seat. Keep your operated leg out straight and lower yourself into the seat bottom first
- Slide your bottom back towards the driver’s seat, a pillow or cushion placed over the handbrake may make this more comfortable
- Gently turn to face the front, keeping your operated leg in front of you and in line with your body
To get out, repeat the above procedure in reverse
You are advised to avoid long journeys for the first three months after your surgery. You shouldn’t travel for more than half an hour without getting out of the car for a break and we recommend that you do not drive for six weeks following your surgery. We suggest that you contact your insurance company before you start driving again and you should be confident to perform an emergency stop.
- You should expect, as with any major operation, to feel tired for the first few weeks
- You should be able to do many of the things you could do before, although it may be a little slower and done in a different way initially
- Allow time for small chores and time to rest
Falling is one of the most common causes of hip fractures. However, you can reduce the likelihood of falling at home by taking the following points into consideration:
- Keep Warm! Muscles that are cold do not work as well and contribute to accidents
- Keep active! Being afraid of participating in activities because you are worried about falling can make you weaker and more at risk of falls
- Clear away loose rugs or tape down the edges
- Clear away cables, wires or any clutter from your walkways, particularly the stairs
- Ensure your home is well lit
- Make sure your footwear is flat, supportive and lace-free if possible
- Get your eyesight checked regularly. Eye tests are free if you are aged 60 or over
- Some medications can make you feel faint or unsteady. Discuss this with your doctor if you are concerned
Therapy department
01935 384 358
Ward 6B
01935 384 272 / 384 820
Ward 6A
01935 384 322
Orthopaedic Outpatient Clinic
01935 384 319
Somerset Direct
0300 1232 224
somerset.gov.uk
Dorset Care Direct
01305 221 016
Red Cross
Equipment loan
0344 8711 111
Text phone 0207 5622 050
redcross.org.uk
NHS 111 service
111
Textphone 018001 111
nhs.uk/111
National Osteoporosis Society
0808 8000 035
nos.org.uk
Age concern
0845 6434 709
ageconcernsomerset.org.uk








