What is a hip arthroscopy?
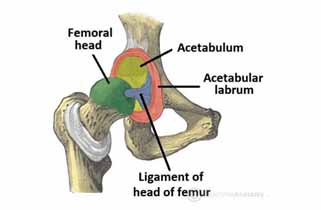
An arthroscopy of the hip is an operation to examine the hip joint under anaesthetic. A small incision is made so an instrument, called an arthroscope (a long thin telescope with a video camera), can be inserted into the hip. The surgeon will examine the joint by looking at images sent by the arthroscope to a computer screen and repair any damaged structures as necessary.
A hip arthroscopy is commonly used to treat labral tears (when the cartilage is torn, or coming away from the hip socket), removal of loose bodies such as cartilage or bone fragments from the joint, and to treat femoral acetabular impingement (FAI) where there is too much friction (rubbing) in the hip joint.
The benefit of operating through small incisions like this is that there is minimal disruption to the surrounding tissues allowing you to progress quickly with rehabilitation and return to normal function as rapidly as possible.
This leaflet will help to explain what you can do to ensure that you have a good recovery and minimise complications. It will also help you understand what to expect and what is normal after a hip arthroscopy. A member of the physiotherapy team will generally see you prior to your surgery to review advice, exercises and to issue you with crutches.
Immediately after theatre
You can start your exercises as soon as you remember to when you return from theatre, you will find them in this booklet. Staff will help you to get up with the crutches when you have recovered sufficiently from the anaesthetic.
Before you are discharged you will be given specific advice about your wound care and pain relief. The leaflet contains general information about this.
Wound care
The small wounds from the arthroscopy will usually be closed with a single stitch and a paper strip. These are covered with a see-through dressing. Do not disturb the see through dressings and make sure that you keep them clean and dry. You will need to make an appointment with your practice nurse 7-10 days after your operation for your wound to be reviewed and stitches removed.
If at any time you notice any discharge, smell, irritation, or redness around the wounds/dressings, you must contact your GP.
Managing your pain
It is likely that your pain will be well controlled immediately post operatively as local anaesthetic is usually placed into the joint during the procedure. It is therefore sensible to take some regular pain relief so that when the local anaesthetic wears off you remain comfortable. Although the hip arthroscopy often helps with the symptoms you have been experiencing your hip will react to the surgery and this can sometimes take a little while to settle down.
Should you experience any increase in pain and swelling not relieved by elevation and rest, or any pain in the calf, please consult your GP.
Managing swelling
Swelling is part of the natural healing process but if it becomes excessive this can lead to increased pain, increased time for wound healing, general discomfort and slower return to activities.
Swelling naturally peaks at 3-5 days following an injury or surgery.
It is strongly affected by gravity and so if you spend a lot of time on your feet then it is likely to increase as a result. Gravity can be used in our favour by elevating the affected limb. We therefore suggest that you pace your activity, especially over the first week after surgery. Try to keep your leg up whenever you sit and try to rest your leg in a position where your foot is higher than your hip for short periods through the day (to aid circulation).
Ice
Ice can be a very useful tool to help with both swelling and pain.
You should be cautious with its use to ensure that you do not damage your skin. We suggest that you follow the precautions below:
- You should ensure that the area to be treated is sensitive to temperature by placing a cold and then a warm object against it and making sure you can tell the difference.
- Use crushed ice, gel packs or even frozen peas as an icepack but always ensure that there are 2 layers of towel between your skin and the ice pack.
- Check the skin beneath the ice pack after 10 minutes, the skin is likely to be red but should not be white or blue. If you are concerned then the ice pack should be removed immediately. If your skin is frail or has poor circulation then you should check it after 5 minutes. If there is no adverse reaction then the pack can be reapplied for a total of 20 minutes
- Ice packs are most effective when applied for 10-20 minutes every 3-4hours.
IF YOU FEEL PAIN AT ANY STAGE ALWAYS REMOVE THE ICEPACK AND CHECK THE SKIN FOR SIGNS OF LOSS OF CIRCULATION E.G. WHITE/PURPLE /BLUE OR VERY COLD SKIN. ICE PACKS USED INCORRECTLY CAN CAUSE ICE BURNS.
Using crutches
You will be issued with and taught to use crutches by a member of the physiotherapy team, usually before your operation. Normally you will place the crutches forward first, followed by the operated leg and then the un-operated one. The nursing staff will ensure you are walking safely with your crutches before you are discharged.
As a general guide you only need to use the crutches for comfort and to prevent you limping (this may be for around two weeks or more). If you decide you only need to use one crutch we advise that you use the one on the side away from the operated leg to keep you well balanced. You should only move on from 2 crutches to 1 crutch or 1 crutch to no crutches when you are able to do so without limping.
The surgeon may ask for you to limit the amount of weight on your operated leg. If this is the case then you will be informed of this and given further instruction if needed. It is very important that you follow this advice if it applies to you.
When going upstairs we suggest that you take one step at a time lead with the UNOPERATED (strong) leg. Follow with the OPERATED leg and the crutch, one step at a time. When going downstairs place the crutch(es) on the step below, followed by the OPERATED leg before bringing down the UNOPERATED (strong) leg to join it.
Always use a hand rail or bannister, if there is one available, during your recovery.
Post-operative follow – up
You should be referred to outpatient physiotherapy around 2 weeks after your surgery. We will usually contact you at home to arrange this appointment within a few days of discharge. The surgeon will usually see you within the first 12 weeks after the operation.
Exercises
It is important to start exercising soon after your arthroscopy to ensure that you return to normal movement, strength and activities as soon as possible. It is important to perform the following exercises 4-6 times per day. We suggest that you exercise little and often throughout the day. Slow controlled exercises are more effective and more comfortable than quick movements. You may experience some discomfort initially with these exercises but it is important not to push into pain. If your pain persists please contact your GP or physiotherapist.
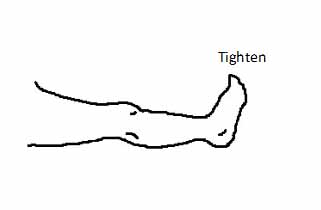
- In sitting or lying with your leg supported, tighten thigh muscles and straighten the knee as far as you can. Repeat 10 times.
2. In sitting or lying with your leg supported, bend your ankles up and down through the full range of movement. Repeat 10-20 times.

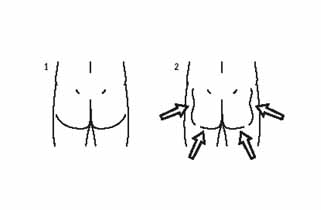
3. In sitting or lying, squeeze your buttock muscles to activate your gluteal muscles. Hold for 3-5 seconds. Repeat 10 times.
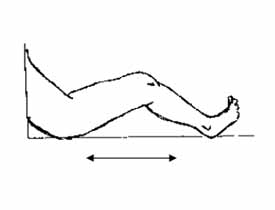
4. Lie with your legs out straight. Gently and slowly slide your heel towards your bottom until it feels tight, then slowly straighten your leg. Do this as pain allows. As your knee bend gets easier you can practice bending your knee while sitting in a chair. Repeat 10 times.
5. In standing, hold onto a support. Standing on your un-operated leg, take your operated leg out to the side. Repeat 10 times.

6. Lie flat with your knees bent and feet supported. Rotate your pelvis towards your belly button. Push your belly button down into the floor (so your back is flat). Rotate the opposite way. Repeat 10 times.

Returning to normal activities:
Driving
People normally return from 2 weeks after their arthroscopy, although this can vary depending on comfort (you may wish to discuss this with your physiotherapist). You have to be able to do an emergency stop in a car to be safe to return to driving. It may be worthwhile contacting your insurance company to find out when they would be happy for you to return.
Work
Your return to work will depend on your job. Please discuss this with your doctor or physiotherapist.
Sport
Your return to sport will depend on the type of activity and the level you play at. Please discuss with your Physiotherapist what sports you can do and when.
Travelling
We advise you to refrain from flying for at least 6 weeks after surgery.
Contact details
If you have a query about exercises or movements, or have not seen a Physiotherapist before being discharged home please contact: Yeovil District Hospital Therapy Department on 01935 384358
Ref:34/20/05
Review:11/22