The shoulder joint
The shoulder is a complex structure that joins the arm to the body. It is made of three bones, including the humerus (upper arm bone), scapula (shoulder blade), and clavicle (collarbone).
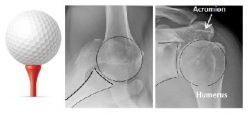
The shoulder is known as a “ball and socket” joint, with a large ball and shallow socket that allows the shoulder to have a larger amount of movement than any other joint in the body. It can be likened to a golf ball sitting on a golf tee.
The joint surfaces are covered by articular cartilage and the joint has a small amount of lubricating fluid. This allows the joint to move effortlessly with more than 100 times less friction than ice moving on ice.
The shoulder relies on surrounding muscles called the rotator cuff to make sure that the “golf ball stays on the golf tee” during shoulder movement.
What is the problem?

As we get older it is common to develop some wear and tear to your joint cartilage. As the cartilage continues to wear, the joint becomes more inflamed and movement becomes less. This causes increasing pain, which can be worse at night.
With worsening arthritis, the pain can get so bad that it interferes with your life. Pain killers may not help anymore and you struggle to do simple activities such as get something from your back pocket or brush your hair. It can also wake you up at night or prevent you from going to sleep.
What are the causes?
For most people there is no obvious cause why the arthritis develops. Factors such as manual work, family history and previous trauma can all contribute. Some patients may have rheumatoid arthritis but most of the time it just happens.
Why do I need an operation?
It is likely that you have already tried non-surgical treatments for your shoulder such as pain killers, lifestyle changes, physiotherapy and injections.
If these measures have not improved your symptoms then the next logical step is to consider a shoulder replacement. This is a major procedure with potential risks and so you need to consider this carefully. When considering any operation it is important for you to weigh up how bad your symptoms are and what an operation can achieve.
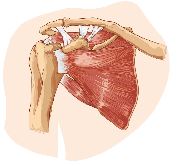
A shoulder replacement is very effective at improving pain. It is also quite effective at improving mobility and function. The shoulder is a complicated joint and relies heavily on the rotator cuff muscles and the muscles around the shoulder blade to achieve the excellent range of movement it has.
A shoulder replacement only replaces the joint and so you have to rely on the muscles to regain their strength to improve the function and mobility. This recovery varies between patients and so there are no real guarantees regarding improving function and mobility.
It is normal, however, for a patient to get their hand behind their head comfortably following a shoulder replacement.
- Constant pain despite taking regular painkillers
- More bad days than good
- Pain that keeps you awake at night
- Difficulty doing your normal, everyday activities or work due to shoulder pain
- Pain and symptoms that come and go
- Not taking regular painkillers
- Able to sleep undisturbed
- Able to work, do daily activities with minimal problems
Deciding whether a shoulder replacement is right for you
If you feel that your symptoms fall more in the first box then a shoulder replacement could be right for you.
If you feel your symptoms are more in the second box it is likely that you will not benefit as much from the operation. If you have not got as much to gain you potentially have more to lose and so it might not be the right time to proceed to a shoulder replacement.
This is a very important decision and so you should take time to consider whether you would like to proceed. Your surgeon will be able to answer any questions that you have.
For more information please read the leaflet linked below:
Before and after your operation
Joint replacement surgery is a major operation and so, as with any major operation, complications can occur.
The vast majority of patients make a good recovery and experience no serious problems after a shoulder replacement operation. However, it is important you understand that complications can occur.
Infection
A deep infection occurs in less than one per cent of shoulder replacements. This is a serious complication but is thankfully quite rare. You are given antibiotics around the time of your surgery to reduce your risk.
If infection does occur you may need to have the shoulder replacement removed, treat the infection using antibiotics and the replace the shoulder at a later date.
Damaging nerves and blood vessels
This, again, is a rare complication (less than one per cent). As surgeons, we know where the major nerves and vessels are and so we aim to avoid them during surgery.
Blood clots
Blood clots in the leg veins (deep vein thrombosis/DVT) and blood clots on the lungs (pulmonary embolus/PE) can occur after shoulder replacement surgery. These are quite rare and occur in less than 0.5 per cent of patients.
You will undergo an assessment to work out your risk for developing blood clots before your surgery and your doctor may prescribe blood thinning medication depending on this assessment.
The simplest way for you to reduce your risk is to keep well hydrated and start mobilising soon after your operation.
Implant wear and loosening
Most shoulder replacements (more than 80 per cent) continue to work well after ten years. However, loosening or wear of the artificial joint can occur. This may cause symptoms of pain and so you should seek advice from your GP or the orthopaedic team if you have new symptoms. Loosening can occur without symptoms and so the orthopaedic team will continue to follow you up with check x-rays for many years after your surgery, even if your shoulder is not causing you problems.
Dislocation
The new prosthetic joint is not as stable as a natural shoulder joint, and it needs to be protected while the surrounding soft tissue structures heal after surgery. You must wear a sling after your operation to allow for this healing to occur. This may be as long as four to six weeks.
Stiffness
The shoulder is an incredibly mobile joint and so it is virtually impossible for a shoulder replacement to achieve the same movement that a healthy shoulder has.
Most people can comfortably get their hand behind their head and behind their back. It takes time to strengthen the muscles around your shoulder and so it may take up to a year to get your final result.
The main reason for having a shoulder replacement is for pain relief. It is likely that you will have some improvement in shoulder function but this is much more difficult to predict and so should not be relied on.
Rotator cuff failure
The rotator cuff muscles that wrap around the shoulder joint are essential for your shoulder to work properly. The operation has to cut one of the tendons to these muscles (subscapularis) to be able to get access to your shoulder joint and this is repaired at the end.
The result of your shoulder replacement depends greatly on whether this tendon heals and so it is essential that you protect this in the first few months following your surgery.
The rotator cuff tendons can also tear years after shoulder replacement surgery. This can cause a loss of movement and pain in the shoulder. The tendons can rarely be repaired if this happens but if your symptoms are bad, your surgeon may consider a revision shoulder replacement.
A total shoulder replacement removes the worn out joint and replaces it with an artificial joint that recreates the shape of a healthy shoulder. The “ball” is replaced with metal and the “socket” with plastic. This combination provides low friction to allow your shoulder to move easily and wear out slowly.
The operation is performed under a general anaesthetic and you will spend three to four hours in the operating department. The operation itself takes approximately two hours.
Once under general anaesthetic, an incision is made at the front of your shoulder. One of the rotator cuff tendons (subscapularis) is cut to allow access to your shoulder joint. This tendon is repaired at the end of the procedure.
The result of your shoulder replacement depends greatly on whether this tendon heals. As stated above, it is vital that you protect this repair for the first three months after your surgery.
Your physiotherapist will advise you how to do this.
Once the shoulder replacement has been inserted and the tendon has been repaired, the skin is closed, normally using an absorbable stitch. A dressing is applied and your arm is placed in a sling.
You will need to use this sling during the first six weeks and so it is important to understand how it works. The nurses and physiotherapists will help you with this.
You will require an x-ray of your shoulder and blood tests after your operation. Your length of stay in hospital depends greatly on how well you feel, whether your pain is under control and what support you have at home. Most people feel able to go home the following day after surgery but sometimes it can take a few more days to feel ready.
You will only be discharged when the physiotherapists and nurses are happy that you will be able to manage at home.

The operation is performed under a general anaesthetic and so you will be given instructions as to when you need to stop eating and drinking (normally the night before) before you come into hospital.
It is common for you to be offered a nerve block to help with the pain. The nerve block allows excellent pain relief immediately after the operation. It is considered a safe method of providing pain relief with few complications (less than one per cent). You will wake up with a numb arm, similar to when you sleep on your arm awkwardly. The block wears off within 12-24 hours and so it is important to take pain killers the night after the surgery even if you don’t have pain when you go to sleep.
The anaesthetist will talk more about the nerve block when they see you. If you do not want a nerve block your pain can be controlled with local anaesthetic given during the operation.
If you smoke, stop smoking. Your chest needs to be clear for the operation. Giving up several weeks before the operation reduces the risk of breathing problems and improves the healing of the body.
Eating a varied, healthy and balanced diet will also help your recovery and healing. For more detailed information please see the NHS Choices website.
Drink alcohol only in moderation. Limit the amount of alcohol to 14 units for women and 21 units for men a week and try to have two days free of alcohol in each week.
Please start thinking about when you go home and start to organise and make the necessary arrangements.
Many patients find it helpful if friends or relatives come to stay, or they go and stay with them following your discharge from hospital.
Convalescence is not funded by the hospital or social services, but you may be able to arrange this privately. Home care is limited and the need is assessed on an individual basis.
You need to consider how you will manage any caring responsibilities you have (including pets), shopping, laundry and meals.
Some pain after your shoulder replacement is inevitable but it is important that we keep this at a tolerable level. You will have regular pain relief medication prescribed for you with access to stronger pain relief if you require them.
Controlling your pain is an essential part of your care and so you must inform the nurses on the ward if you feel that your pain is not controlled.
You will be asked to describe your pain on a scale of 0 – 10, zero being no pain and ten being the worst pain you have ever had.
You can also be referred to the pain specialist nurse if your pain is difficult to manage.
The new replacement joint is not as stable as a natural shoulder joint, and it needs to be protected while the surrounding soft tissue structures heal after surgery.
You must wear a sling as instructed to do so.
You will be advised which movements you must not do and which exercises you should do.